“They come out with chocolate.”
She was right. The patient produced a chocolate bar, waved it in front of her index finger, and a small, worm-like creature wiggled out of her fingertip.
I might not have believed it if I didn’t see it with my own eyes, and in fact, several other clinicians didn’t believe it when she brought the concern to them, either. Urgent care advised emollients to treat her dry, cracked skin. Emergency advised a psych consult. But you and I know, all roads lead to primary care, and that is how this patient and her passenger ended up with us that day.
She wasn’t my patient; she was the last patient of the morning session, there to see a colleague of mine. That colleague came out of the exam room looking for another set of eyes — and hands.
Seeing is believing. The patient said that she had been eating chocolate when she first noticed something working its way out of her fingertip toward the candy. She couldn’t tell what it was, and it went away when the candy did. Her hands were very dry, and her fingertips were cracked longitudinally. Other than the dry, cracked skin, I didn’t see anything remarkable on her hands; no blisters, no erythema, no crusting or drainage, no rash. The nails were trimmed and appeared clean. But when that candy bar came out, so did … something.
I looked through my bifocals and the headband magnifier while my colleague held a light to the patient’s fingers. Something began to poke out. “Keep the candy right there,” one of us advised. With an open spec cup in one hand and the forceps in the other, it took me three tries to grab it, then I lost my hold and it retreated. The candy bar was waved again, and we waited a moment for it to reappear. I was ready this time, and successfully pulled it out without crushing it.
We sealed the cup and labeled it. The wiggly thing looked like a tiny grain of rice. What was this?
The spec cup went off to pathology, and I went on with my day. Maybe a week later, the report came back; I recall it being something like a mite. My colleague referred the patient to dermatology, and the final verdict was that this mite (or similar) had hopped from the patient’s dog (who slept in her bed) and burrowed into her fingertip. Dermatology started treatment for the patient, and advised her to follow up with her vet for the dog’s treatment.
This didn’t happen overnight. The patient had sought help and treatment from several clinicians. It isn’t fair to say that she was dismissed, but she was sent in directions that were ultimately not fruitful for her and that did not definitively treat the issue. Were we heroes in primary care for being able to get her on the right path to resolution? No. We were lucky. We happened to have a little bit of extra time and a set of extra hands to get a sample to identify.
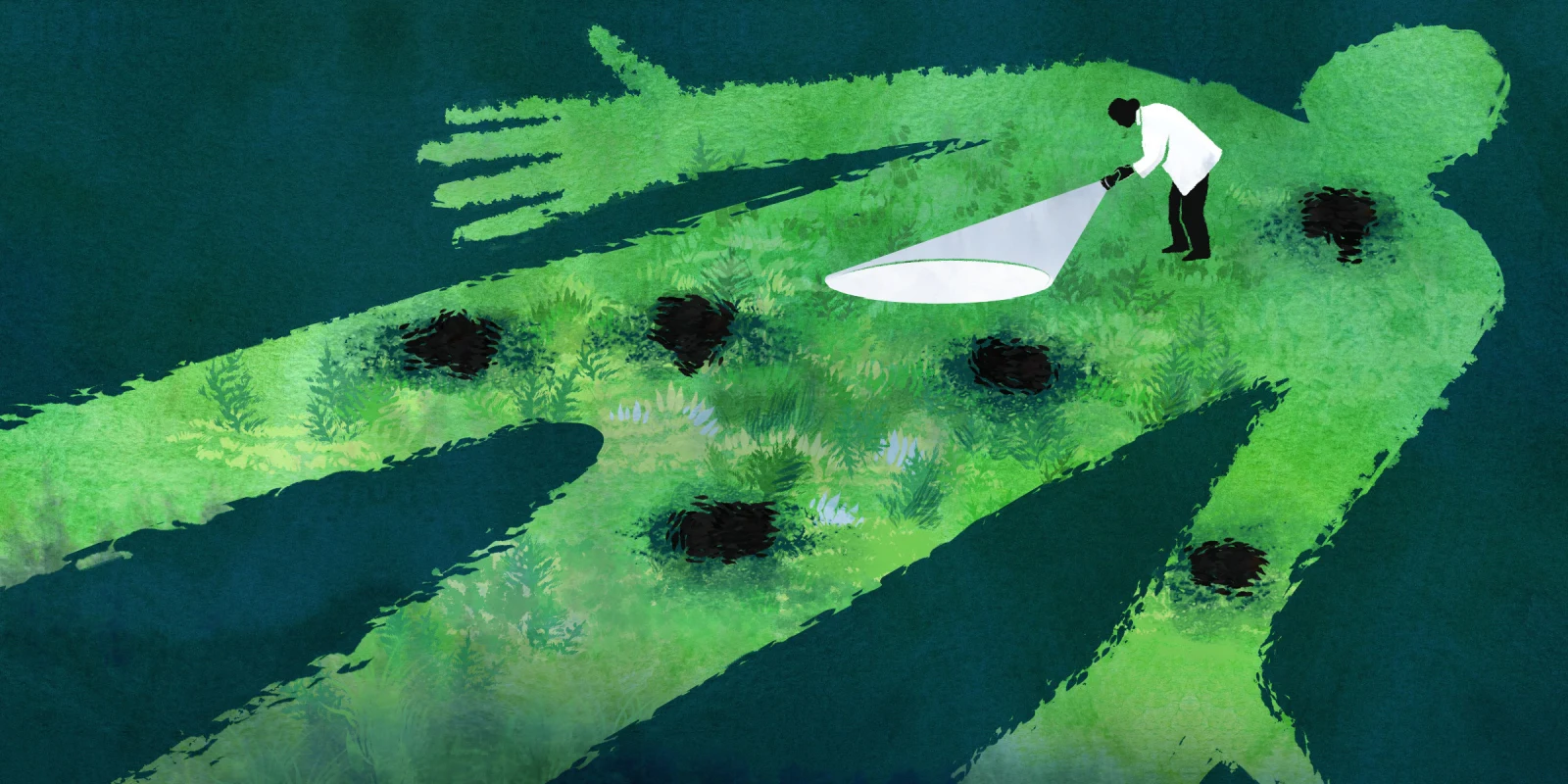
There is not an abundance of literature on what happens when patient concerns are dismissed or incorrectly attributed to another cause. A large study completed in 2015 focused on second opinions, and the prevalence of change to diagnosis and/or treatment plans based on patient-initiated second opinions. Of nearly 7,000 cases included in that study, approximately 15% resulted in a change of diagnosis, and 37% in a change of treatment plan (another 10% with both a change in diagnosis and treatment). Those are compelling numbers, though there are some caveats: participants in this study were part of a free program offered by their health insurance company. It begs the question about patients with similar concerns with different health insurance coverage and how they go about getting their diagnosis on issues big and small. In the case of rare diseases, another study showed that patients visit an average of six physicians before receiving their diagnosis; it’s not uncommon for these patients to spend years searching for a diagnosis.
What if the patient had her appointment scheduled for 10 a.m. instead? A second set of hands might have been much harder to come by. What if the patient went with the psych consult that was suggested by emergency? What if my colleague chose to prescribe antibiotics or a steroid, thinking this was dermatitis? Having the time to fully investigate what the patient had been experiencing, having the capacity for suspension of disbelief while the patient lured the interloper out with some candy, having the luxury of a second set of hands and the right slot in the schedule — all of these things came together to get this patient her diagnosis.
While I got an interesting story out of it, years later I still can’t help but wonder what if? What if this could have been caught sooner? What if we weren’t able to get the specimen? What if she hadn’t come to our office that day?
We learn in school, “If you hear hoofbeats, think horses, not zebras.” For the large majority of our patients and their clinical presentations, this is good advice. And usually those longshot “zebras” are once-in-a-career clinical presentations or constellations of symptoms that may make a great story or focus for research, but that might not change our routine practice by much. What about the patients, like this one, who aren’t quite horses or zebras? Should we focus on something other than the metaphorical hoofbeats — and if, so, what? Or is it more accurate to say recognizing the “not horses or zebras” is something that develops over time as we add years to our practice, almost a rite of passage? On paper, that sounds great, but what about the patients who have to experience the relay race of health care, with multiple visits before getting a definitive diagnosis and treatment?
I would like to be able to say that this changed the way that I practice, but it hasn’t. Though it has made me question the way that we work with patients, and the amount of weight we give to their stories. Sometimes seeing is believing.
What non-zebra and non-horse diagnosis sticks in your brain? Share in the comments.
Jessica Reeves is a nurse practitioner as interested in the well-being of her fellow clinicians as that of her patients — and she's on a mission to make the work world a better place to live. She writes, works, and lives in the town that holds the world record for most lit jack-o-lanterns (really). Follow her at jessicareeves.net. Jessica is a 2023–2024 Doximity Op-Med Fellow.
Illustration by April Brust