As a practicing psychiatrist I’ve met many pregnant physicians seeking additional emotional support amidst conflicted feelings about balancing career and family. A common complaint revolves around the transition of identity; physicians who have unilaterally identified themselves through their careers typically have extraordinary struggles incorporating motherhood into their self-identity. Many describe feelings of guilt around taking time off for their prenatal appointments or for their perceptions of creating more work for their colleagues. Yet others fear that pregnancy, maternity leave, and the demands of family will prevent them from achieving the career heights they would have otherwise. Fortunately, supporting our pregnant colleagues is an opportunity to improve their wellbeing and pregnancy outcomes, promote equity and good morale in the workplace, and retain high levels of medical talent and leadership.
Many female physicians pursue pregnancy at some point during their training or careers. Physician pregnancies are fairly common, given that women often attend medical school and residency during part of their reproductive span. Since women constitute one third of the physician work force and over half of all medical school classes, it’s increasingly important to consider how best to support pregnant physicians when designing programs and workplaces.
You’re Pregnant. What Will Your Colleagues Think?
Recent studies have shown that female physicians provide care that is at least equal to or even better than their male colleagues in many circumstances. Despite that, female physicians have been significantly impacted by work inequities, often getting promoted less, being in fewer leadership roles, and making less money.
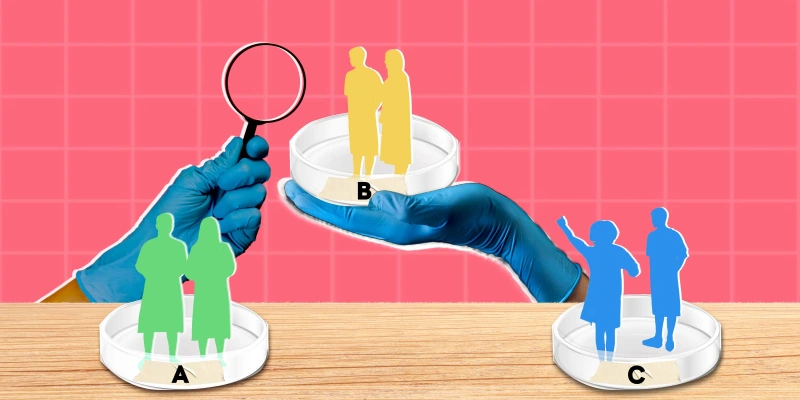
Female physicians who opt to pursue pregnancy during their careers often cite conflicted feelings about balancing their careers and family planning. These conflicted feelings can be worsened by the perception that their colleagues have negative attitudes towards this decision. The perception of female physicians has been that their male and female colleagues, administrators, and their superiors have had negative attitudes towards their childbearing, particularly during medical school and residency. Many female physicians report that they had a negative experience being pregnant during residency. An older study also revealed that physicians viewed their pregnant colleagues as significantly less dedicated to or interested in their medical practices. Fortunately, these attitudes have slowly and progressively improved over time.
Are Physicians at Risk for Poor Pregnancy Outcomes?
A common concern is that the unique stressors experienced by pregnant physicians might have a negative impact on the outcome of the pregnancy.
The data on outcomes of physician pregnancies is limited and conclusions about such are often conflicting. Still, there is no definitive or consistent data that physician pregnancies result in higher rates of poor outcomes. This was even true for proceduralists, those with toxic exposures, and those with extended work days. However, because of long hours, strenuous physical demands, and high levels of stress, pregnant physicians may still benefit from being managed as a higher risk group.
Physicians are notorious for poor self-care, with a recent report even suggesting that 80% of physicians work through illnesses for which they believe others should be excused from work duties. A self-report comparing the experiences of pregnant female physicians to their non-pregnant female physician peers reveals that pregnant physicians enjoy a better health status, equal exercise and more fruit and vegetables intake than their non-pregnant physician colleagues.
6 Tips for Improvement
How can we be supportive of our pregnant physician colleagues, employees and trainees? Here are some tips to consider:
1. Encourage safe workplace precautions. Although safety precautions are important for all physicians, immune system changes make these especially necessary for protecting the pregnant physician and her child. For example, the utilization of standard precautions against infections (i.e. well-fitting N95 masks, gowns, handwashing, and body fluid isolation) may be particularly protective. This is also an opportunity to review the practice’s policies for minimizing toxic exposures and encouraging other safe workplace practices.
2. Have clear maternity/paternity leave policies. Setting consistent expectations around maternity/paternity policies for a pregnant physician will be important as she makes her plans. This will reduce any questions or misconceptions and help the pregnant physician in setting up her childcare and in easing her transition back to work after her maternity leave.
3. Proactively plan how to cover the work gaps during the doctor’s leave. A prolonged leave of any kind can create logistical issues for the remaining workforce. Whether it is by hiring temporary providers or fairly redistributing the extra load across the existing workforce, coming up with a proactive plan early on will be important in ensuring there are no gaps in coverage. A fair plan could reduce concerns that the other physicians will have to work overtime to cover the patient load and may be important for the overall morale of the pregnant physician and the remainder of the group.
4. Encourage good mental health. Physicians often cite stigma as a primary reason for avoiding mental health treatment, even when struggling with severe symptoms. Physicians are not immune to perinatal mental health difficulties, although they may be more inclined to try to “power through” their symptoms instead of seeking treatment. Don’t be afraid to lend some support or a listening ear to a colleague who looks like she is having a hard time. Mental health treatment during this timeframe can be crucial in some cases, and those who are surrounded by people who are supportive of it may be more inclined to seek this treatment.
5. Postpartum support. Many physician mothers report that they have prematurely discontinued breastfeeding and pumping due to a lack of departmental support, insufficient time, and no private space in which to do so. A protected place for breastfeeding/pumping breast milk may be mandated by your state policy, and providing this space could support a mother in her choice of healthy postpartum practices.
6. Explore our own biases. As the physician workforce grows increasingly diverse, we will need to explore and be aware of our own biases towards physicians who plan to pursue childbearing. Although the prejudices and misconceptions against pregnant physicians by their colleagues certainly seem to be improving, any remaining prejudices could impact the morale of the pregnant physician and may impact important decisions, such as whether to promote the physician to leadership positions.