Seated in front of me, Casey looked much more relaxed than she had in the hospital. Her makeup was done, and her smile was wide. When we first met, she was recovering from a serious lung injury caused by vaping, the term commonly used for e-cigarettes. She needed ICU-level care and high doses of steroids to reduce her lung inflammation. But now that she was out of the hospital, she didn’t hesitate to share her story.
“All my friends were vaping,” she said. “So I did it too.”
She told me she suffered from both anxiety and depression. The experience of being treated for severe lung injury from vaping in the hospital scared her enough to quit. But then she added with a shrug, “Everyone at the club still does it.”
That line echoes what I’ve heard from so many patients: everyone vapes. They do it in school bathrooms, on campus, even in their bedrooms. Many teens start because a friend or family member uses it, or because they’re drawn to the unique fruity flavors. But what’s most disturbing is how unaware most parents are of how common adolescent vaping has become and how dangerous it is. I wish more parents and doctors knew how to talk to kids about vaping.
When I talk to teens, I try to bring up vaping in a nonjudgmental way: “A lot of kids are vaping. Do you know anything about it?” Nearly every teen I ask knows that e-cigarettes are harmful to their lungs — a clear sign that public health messaging is working. I make sure to applaud them for their awareness. But that’s usually when a parent jumps in with, “Oh, she would never try that stuff,” or, “He knows better than to use those things,” accompanied by a threatening glare. My patients look down, uncomfortable and silent.
We need a different approach from both parents and clinicians, grounded in facts and free of judgment. The American Academy of Pediatrics recommends that clinicians begin asking about tobacco and vaping use at age 11, as there are some reports of kids starting vaping this early. It’s also recommended to provide patients and caregivers with facts about the harms of e-cigarettes.
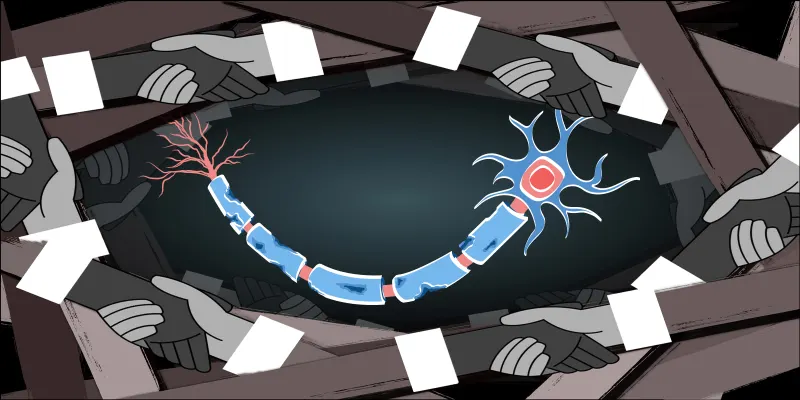
They usually contain an active ingredient such as nicotine or tetrahydrocannabinol (or THC, the psychoactive ingredient in marijuana), and the aerosol produced by vapes contains heavy metals, carcinogenic organic compounds, and other toxic chemicals. Although these toxins are lower in quantity compared to regular combustible cigarettes, vaping is associated with an increased risk of future cigarette use, especially for those who start vaping before age 18. We also know that vaping aerosol causes lung cytotoxicity and is linked to conditions like asthma and bronchitis in adolescents.
Many pediatricians aren’t trained to disseminate this information, and it’s not really their fault. E-cigarettes hit the U.S. market in 2007, but their popularity exploded between 2011 and 2019. By 2019, over a quarter of high school students reported current use. The rates have since declined, but the numbers remain staggering — over 2 million middle and high schoolers in the U.S. still report vaping. Adding to the challenge is the fact that adolescents may not be forthcoming about vaping habits during relatively short appointments with their clinicians, especially with parents around.
This makes it even more critical for clinicians to stay informed because while overall vaping rates may be declining, the landscape of e-cigarettes and related products is rapidly evolving. Today’s vapes may be more addictive. They contain synthetic nicotine and synthetic THC — potent, unregulated, and specifically designed to appeal to adolescents. At a recent medical conference, I was stunned to hear a speaker say that many e-cigarettes contain as much nicotine as 12 packs of cigarettes. The health effects of synthetic THC, which can include psychosis, are only recently being studied.
We need to talk to kids before they initiate e-cigarette use. I felt this strongly last year when I visited my son’s elementary school for career day and asked a bunch of fifth graders, “Who knows what an e-cigarette is?” Every hand went up. They’d seen ads online. One child said, “My cousin vapes all the time.” Some had parents who used them, and when parents use vapes to quit smoking, they send an unintended message to kids that vaping is safer and therefore OK. But no amount of vaping is safe for a nicotine- and tobacco-naïve adolescent.
This is where physicians come in. We have to talk to both teens and parents. We can’t let up just because e-cigarette, or vaping, product-induced lung injury (known as EVALI) cases have declined, because cases still occur, and the potential for health risks is high. Moreover, the vaping industry is moving faster than we are, marketing novel products that kids are trying. We need to make vaping a core topic in medical school and residency training and ensure that pediatricians and physicians feel equipped to counsel on it.
I believe my patients when they say that everyone is doing it. Once a teen starts vaping, it can be very difficult to help them stop, mostly because the addiction potential for adolescents is high, and we still don’t have evidence on what works best to help them quit.
Thankfully, my patient Casey has stopped vaping, but it took an ICU stay for her to realize just how dangerous e-cigarette use could be. In social settings, she’s still surrounded by friends who vape. So I’ll keep talking to her in a non-judgmental way. I’ll continue to make sure she knows the facts about vaping. I have to believe that checking in with my patients, continuing to offer facts, and creating a safe space for candid conversation may help to prevent a lifetime of addiction.
Do you have experience counseling patients on e-cigarette use? Share in the comments!
Devika Rao is a practicing pediatric pulmonologist in Texas. She enjoys writing, trying new vegetarian recipes, yoga, and spending time with her two boys and husband. Dr. Rao is a 2024-2024 Doximity Op-Med Fellow.
Image by ilkov_igor / Shutterstock