On April 24, 2020, the CDC answered questions for Doximity members on PPE, health care provider safety, and system-level strain related to COVID-19. We spoke with two CDC expert physicians. Neil Gupta, MD, MPH, is the team lead of the Health Systems and Worker Safety Team and the CDC COVID-19 Response Team. He is also the branch chief of Epidemiology and Surveillance, a Division of Viral Diseases. Arjun Srinivasan, MD, is the team lead of the Out of Hospital Team, Healthcare Resiliency Task Force, and National Response Coordinating Center Captain at USPHS. He is also the Associate Director for Healthcare Associated Infection Prevention Programs, a Division of Healthcare Quality Promotion.
Read what Dr. Neil Gupta and Dr. Arjun Srinivasan had to say about PPE, health care provider safety, and system-level strains.
Doximity: Are there specific self-protection recommendations for higher risk health care employees (those pregnant, over 50, going home to families with higher risk members)?
Neil Gupta, MD, MPH: As with all health care personnel, we want to be sure providers are being as safe as possible when caring for patients. Health care personnel at higher risk should talk with their supervisors to identify roles that would put them at lower risk of exposure to COVID-19 patients.
Doximity: Why isn’t the CDC setting firm/universal standards around PPE for providers caring for suspected Coronavirus patients?
Neil Gupta, MD, MPH: Health care personnel and first responders are the heroes of this epidemic working on the front lines to save lives every day, and we want to ensure they remain safe when caring for patients with suspected or confirmed COVID-19. CDC has worked with stakeholders across the health care system to identify infection prevention and control strategies that balance the need to maintain a functional health care system with ensuring health care workers’ safety.
Our guidance is continually updated with the most recent scientific evidence available to ensure health care personnel are safe. However, given the realities of this outbreak, we know health care facilities are increasingly unable to procure reliable and sufficient supplies of personal protective equipment, or PPE. To ensure health care personnel remain safe when interacting with patients, CDC recommends the use of an N95 respirator or a higher level respirator when caring for suspected or confirmed COVID-19 patients. We also recognize that supplies of N95s and other respirators are lacking in many facilities, so we recommend that health care personnel wear a facemask when seeing patients if respirators are not available.
As with the community face covering guidance, CDC also issued guidance that health care personnel and visitors should use “source control” at all times in the facility, which is intended to prevent someone who is infected (asymptomatic or symptomatic) from transmitting COVID-19 to susceptible people whether a patient, visitor, or health care personnel. Patients should use source control upon arrival to the facility, and anytime they are outside their rooms or around others.
Doximity: Some facilities are telling clinicians to only use one set of PPE per 12 hour shift. All patients with cough are given a mask as well. What is the advice of the CDC? How often should PPE/masks be changed?
Neil Gupta, MD, MPH: Ideally, all health care personnel should have access to the proper PPE when and where they need it when for caring for patients. However, as this pandemic has shown us, we are not operating in the ideal scenario. CDC is recommending PPE optimization strategies to help facilities consider the best way to manage PPE use to ensure health care personnel remain safe and that facilities can maintain supplies of PPE for necessary procedures for as long as possible. For example, CDC guidance emphasizes strategies to optimize the current supply of N95 respirators, including the use of devices that provide higher levels of respiratory protection (e.g., powered air purifying respirators) when N95s are not available. We hope that facilities will refer to this guidance and employ strategies that will protect health care personnel and ensure they have access to PPE when needed. We encourage facilities to start using these optimization strategies now if they have not already.
And as I mentioned previously, we are asking all persons, including health care personnel, patients and visitors, to use source control at all times in the facility. Patients should use source control upon arrival to the facility, and anytime they are outside their rooms or around others. health care personnel should wear an N95 respirator when caring for patients with confirmed or suspected COVID-19, particularly during aerosol-generating procedures.
Doximity: How long should exam rooms be left vacant after a patient with URI symptoms after cleaning?
Neil Gupta, MD, MPH: Although spread of COVID-19 is believed to be primarily through respiratory droplets, we’re not sure yet how much these small particles transmit the virus in close proximity. However, we do think that airborne transmission from person-to-person over long distances is unlikely. We don’t yet know the amount of time that the air inside an examination room remains potentially infectious, and it may depend on various factors like room size, how long the patient was in the room, if they were coughing or sneezing, or if an aerosol-generating procedure (AGP) was performed in that room.
In rooms where a patient was not coughing or sneezing, an AGP was not performed, and the room was only used for a short period of time, any risk to HCP and subsequent patients likely dissipates over just a matter of minutes. However, for a patient who was coughing and remained in the room for a longer period or underwent an aerosol-generating procedure, the risk period is likely longer.
For these higher risk scenarios, it is reasonable to apply a similar time period as you would for other airborne pathogens such as measles or tuberculosis, and to restrict HCP and patients without PPE from entering the room until enough time has gone by for air changes in the room to remove potentially infectious particles. HCP should also clean and disinfect environmental surfaces and shared equipment before the room is used for another patient.
Doximity: A potential reason why COVID-19 is spreading so quickly is that the transmission can occur before symptoms are present. Monitoring staff doesn’t address this. Can this be addressed through the use of masks and gloves even when asymptomatic? Are there any safeguards in these instances that might reduce transmission rates?
Neil Gupta, MD, MPH: Asymptomatic transmission continues to be an important factor in this outbreak, highlighting the importance of reinforcing key principles of infection control like maintaining social distancing as much as possible, practicing good hand hygiene, keeping a clean environment, and avoiding touching your face. All of these are safeguards that prevent transmission, regardless of whether you are symptomatic or asymptomatic. Also, CDC’s recently released guidance for the general public on community face covers addresses source control methods, like having everyone wear a cloth face cover when leaving the house, and will hopefully minimize the potential for asymptomatic carriers to shed virus when they go about their daily lives or even enter the hospital ER or waiting rooms. Similarly, CDC is now recommending universal source control for everyone entering a health care facility, regardless of symptoms. This includes patients, visitors, and health care personnel. Although gloves are one part of the personal protective equipment ensemble recommended for health care personnel caring for patients with known or suspected COVID-19, universal glove use is not recommended. However, practicing appropriate and frequent hand hygiene remains a cornerstone of infection control practices.
Doximity: Given the current crisis and unprecedented shortage of data and resources, is the CDC changing standards for PPE?
Neil Gupta, MD, MPH: Protecting health care personnel is a top priority for CDC, and we want all health care personnel to remain safe and healthy when caring for patients during this time. CDC has not changed standards for PPE, and recommendations for proper PPE use can be found here and in CDC’s COVID-19 Infection Control Guidance. However, in recognizing that recommended PPE may not be available, CDC has also provided optimization strategies, found here, for facilities experiencing a shortage of PPE supplies or difficulty obtaining PPE. Proper PPE use is critical to ensuring health care personnel and patient safety. Given the strain that facilities are experiencing with PPE, CDC has and will continue providing resources to health care personnel and health care systems to aid in planning to mitigate these challenges and optimize supplies of PPE. CDC has issued various resources to help facilities to plan to optimize their PPE supplies to ensure that health care workers have access to N95s, gowns, facemasks, and eye protection when needed. We also released a PPE Burn Rate Calculator to help facilities make informed decisions and apply appropriate optimization strategies to help health care systems during this crisis.
Doximity: There has been a lot of discussion on preserving PPE, but yet it’s also been stated that anyone with mild symptoms should be put on droplet precautions. Can the CDC clarify who and which patients need to be isolated and under what level of precautions?
Neil Gupta, MD, MPH: CDC recommends that when caring for any patient with suspected or confirmed COVID-19, even if symptoms are mild, the health care provider should follow Standard Precautions and appropriate Transmission-Based Precautions, which includes the use of a respirator (or facemask if a respirator is not available), gown, gloves, and eye protection. Any patient with suspected or confirmed COVID-19, regardless of symptoms, should ideally be placed in single-person room with door closed and dedicated bathroom.
Doximity: Many patients in long term care facilities are due to be seen by their clinicians (but may not have acute needs). Any guidance on whether regulatory requirements (visiting patients every 30 days for the first 90 days, then every 60 days for the first 90 days) are going to be relaxed?
Arjun Srinivasan, MD: Ensuring nursing home residents can continue to get the care they need is a priority. Many providers have expanded their use of telemedicine to continue to safely care for their patients. Nursing homes should explore the availability of telemedicine options.
Doximity: How can facilities better prepare for significant strains on resources and available patient care space? With the inevitability that health care providers will become sick, how can facilities better prepare for staffing shortages? Are there opportunities for non-medical personnel to assist in patient care?
Arjun Srinivasan, MD: We recognize the importance of planning during this unprecedented situation. As mentioned, CDC has issued PPE optimization strategies for use when PPE supplies are stressed, running low, or absent. All U.S. health care facilities should begin using PPE contingency strategies now to help stretch PPE supplies. Crisis strategies can be considered during severe PPE shortages and should be used with the contingency options to help stretch available supplies for the most critical needs. As PPE availability returns to normal, health care facilities should promptly resume conventional practices. health care personnel and facilities—along with their health care coalitions, local and state health departments, and local and state partners—should work together to develop strategies that identify and extend PPE supplies, so that recommended PPE will be available when needed most.
Over the past several weeks, CDC has also enhanced CDC’s National Healthcare Safety Network (NHSN) reporting system to monitor and analyze the capacity of the domestic health care system daily so that federal, state, and local officials can adjust their response efforts, as needed. Understanding how COVID-19 impacts the capacity of the U.S. health care system is essential for the response to the pandemic. All levels of government, and the nation’s health care system, need detailed and timely information about the availability and shortages of key resources, including hospital beds, ICU beds, ventilators, personal protective equipment, and health care personnel.
NHSN’s new COVID-19 elements aim to minimize reporting burden on the hospital system. Almost every hospital in the nation and thousands of other facilities — over 22,000 total health care facilities in total — use NHSN daily for non-COVID-19 reporting. As of April 20, 2020, more than 3,400 facilities have reported data to the new NHSN COVID-19 module, representing about 52% of general acute care and critical access hospitals. Ongoing outreach efforts continue to increase participation. We thank hospitals for this crucial information, and we thank state and local health departments and partner organizations for their assistance in encouraging this reporting and putting the data to use.
This interview was conducted by Liz Jung, MBA, Business Development Manager and Erin Mercer, MBA, MA, Clinical Content Editor.
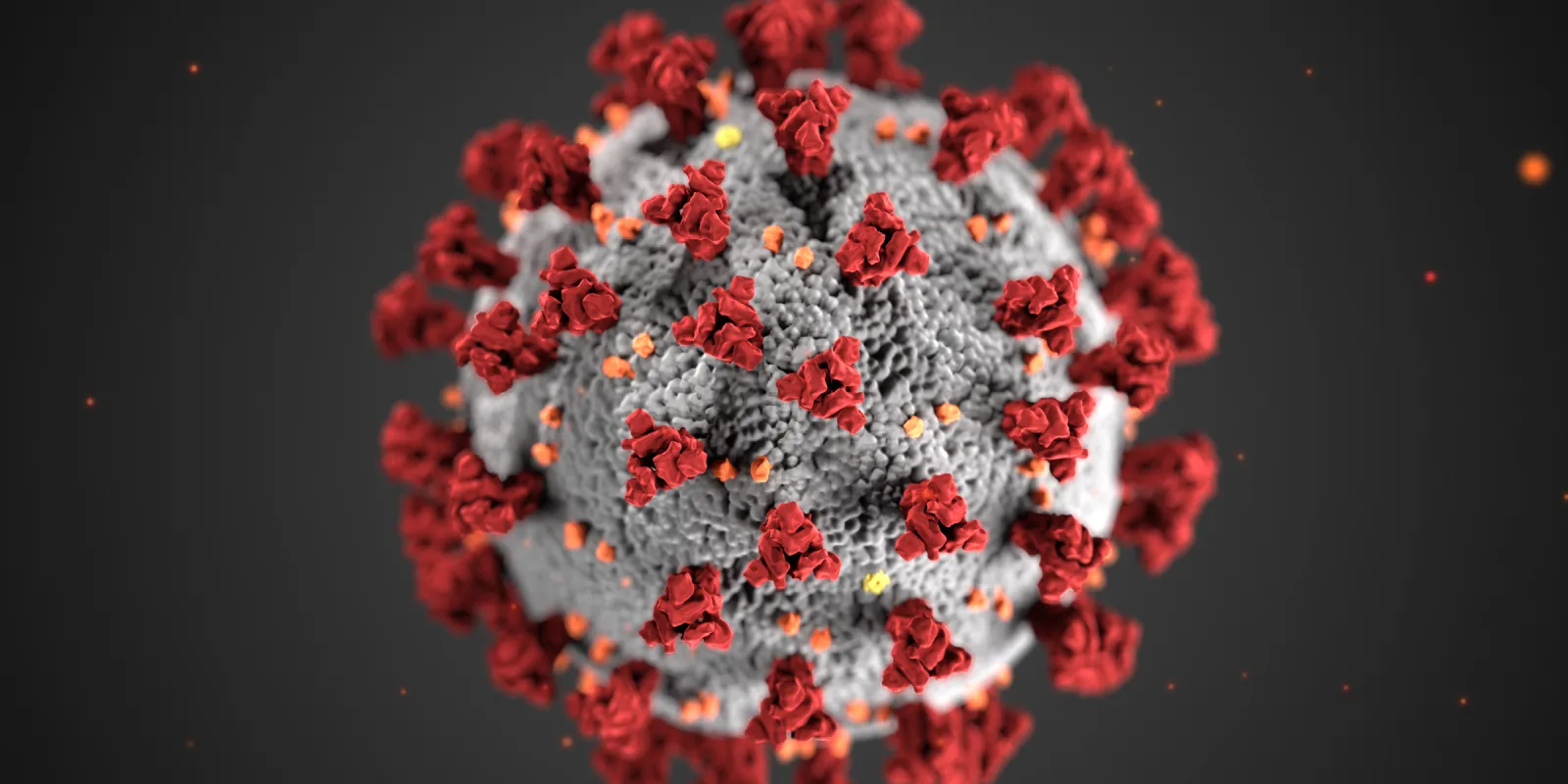
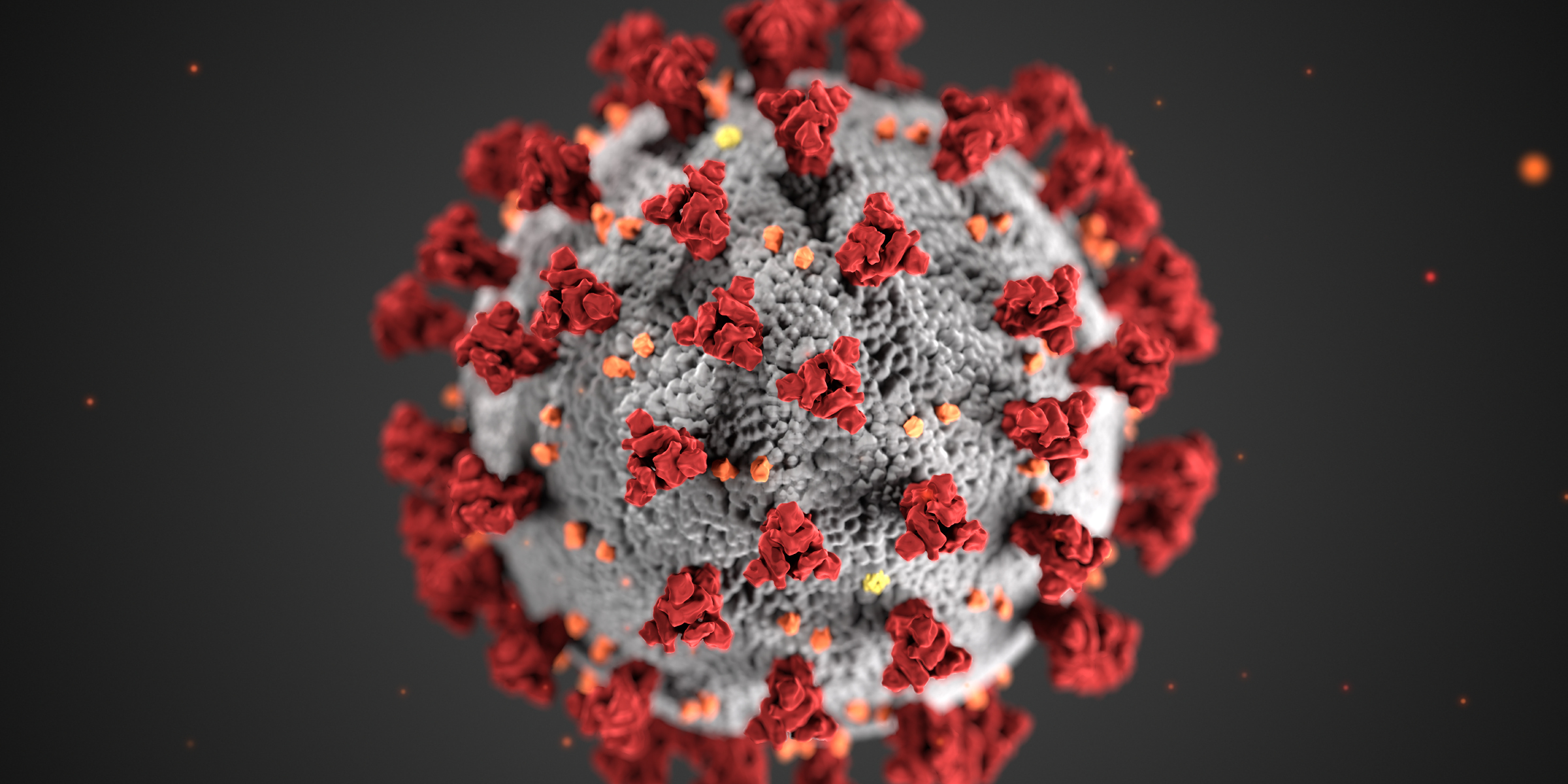
Image via CDC