I am very excited about my Digestive Diseases Week lecture on cancer ablation this year. Cancer ablation is still in its infancy. The lecture will first review the fact that in medicine — often technological innovation — precedes clinical innovation.
For example, nuclear magnetic resonance was first described in 1948, and it took MRI till the 1980s to enter clinical practice. Today, MRI is so integral to our clinical care that it is hard to imagine a time when it was unavailable. Similarly, ablation specifically for cancer is now in its discovery phase, with many technologies available today and many more coming down the pipeline. Research on clinical outcomes is increasingly developing to understand the impact of ablation on cancer treatment and management paradigms.
Another reason ablation is likely to take a more significant role in the future is the genetic diversity of cancer. Gastrointestinal luminal cancer is significantly genomically more diverse than its metastases. This means that as systemic therapy is continuing to become more effective, we are more adept at killing the metastatic and need to augment our antitumor effect locally with another modality. Traditionally the local modality has been radiation, surgery, or a combination thereof. Surgery alters the gastrointestinal tract and disturbs the harmonic symphony of food propulsion and digestion in such a way that the patient’s long-term quality of life is significantly impaired. This is clearly documented in esophageal and rectal surgeries. This has led to a quest by oncology to look for organ preserving strategies to avoid surgery.
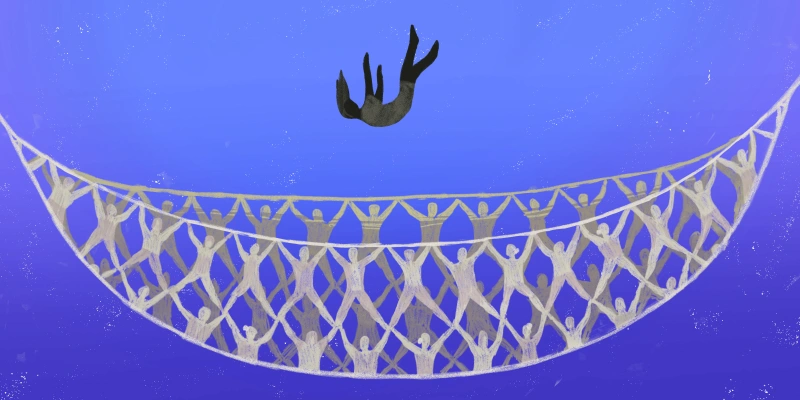
Significant strides in organ preservation have been made, particularly in rectal cancer. Similarly, because of the long-term impact of radiation on the GI tract, oncologists are looking at treatment options that avoid radiation. GI cancer ablation has the potential to replace both radiation and surgery in situations where there is a need to augment systemic therapy with local therapy. Ablation has the advantages of efficacy and safety, especially since ablation can be very selective in creating tissue damage. Therefore, it is significantly more tolerated than either radiation or surgery.
Another area where ablation could be used to add to multimodality treatment is in combination with radiation and/or surgery. Pilot studies are starting to emerge in this field for esophageal cancer. Finally, ablation is starting to be established as a modality for definitive cancer treatment in certain areas, such as pancreatic neuroendocrine tumors. A very exciting area is the impact of ablation on the tumor microenvironment and possible immune modulation, thereby making the tumor more responsive to immunotherapy. This has the potential to impact cancers locally and systemically via the abscopal effect. This will be a paradigm shift in cancer care, making the gastroenterologist a valuable member of the multidisciplinary cancer team.
You can see why I am very excited about my talk, cancer ablation, and the future of gastroenterology’s role in cancer care. As the founder and chair of the Endoscopic Oncology Special Interest Group for the American Society of Gastrointestinal Endoscopy, I have made it my mission to promote research and education in this field. This talk will stimulate people’s interest and catalyze endoscopic oncology.
Dr. Kachaamy reports payments from Boston Scientific, Olympus, Steris, and Medtronic as well as several patents.
Image by BRO Vector / GettyImages