Stem cell transplantation has been considered the standard of care for the management of multiple myeloma for more than 40 years. However, stem cell transplant is toxic with a significant infection rate during the period of maximal myelosuppression. There is also a significant decline in quality of life related to therapy-induced mucositis and the profound fatigue following transplant that can last from 3 to 6 months. The procedure can only be done in highly specialized centers and often requires patients to relocate from home for a period of 6 weeks. For those employed there is also the economic loss associated with the inability to work.
The survival benefit of transplant has been demonstrated in a phase 3 trial. However, these results predate the introduction of lenalidomide and bortezomib as standard induction therapy for patients with multiple myeloma. Over the past 10 years, routine maintenance therapy has been demonstrated to improve progression-free and overall survival for patients with multiple myeloma. It is therefore reasonable to ask whether during the era of novel agent induction and routine maintenance therapy whether stem Cell transplantation continues to provide benefit for newly diagnosed patients with multiple myeloma.
This specific question was addressed at the American Society of Clinical Oncology plenary session on 6/5/2022. The determination trial led by Paul Richardson of Dana-Farber Cancer Institute attempted to address this question in a multicenter phase 3 clinical trial. The fundamental question asked by this trial was how much first-line autologous stem cell transplantation enhances outcomes in newly diagnosed multiple myeloma or can stem cell transplantation be delayed without compromising outcomes?
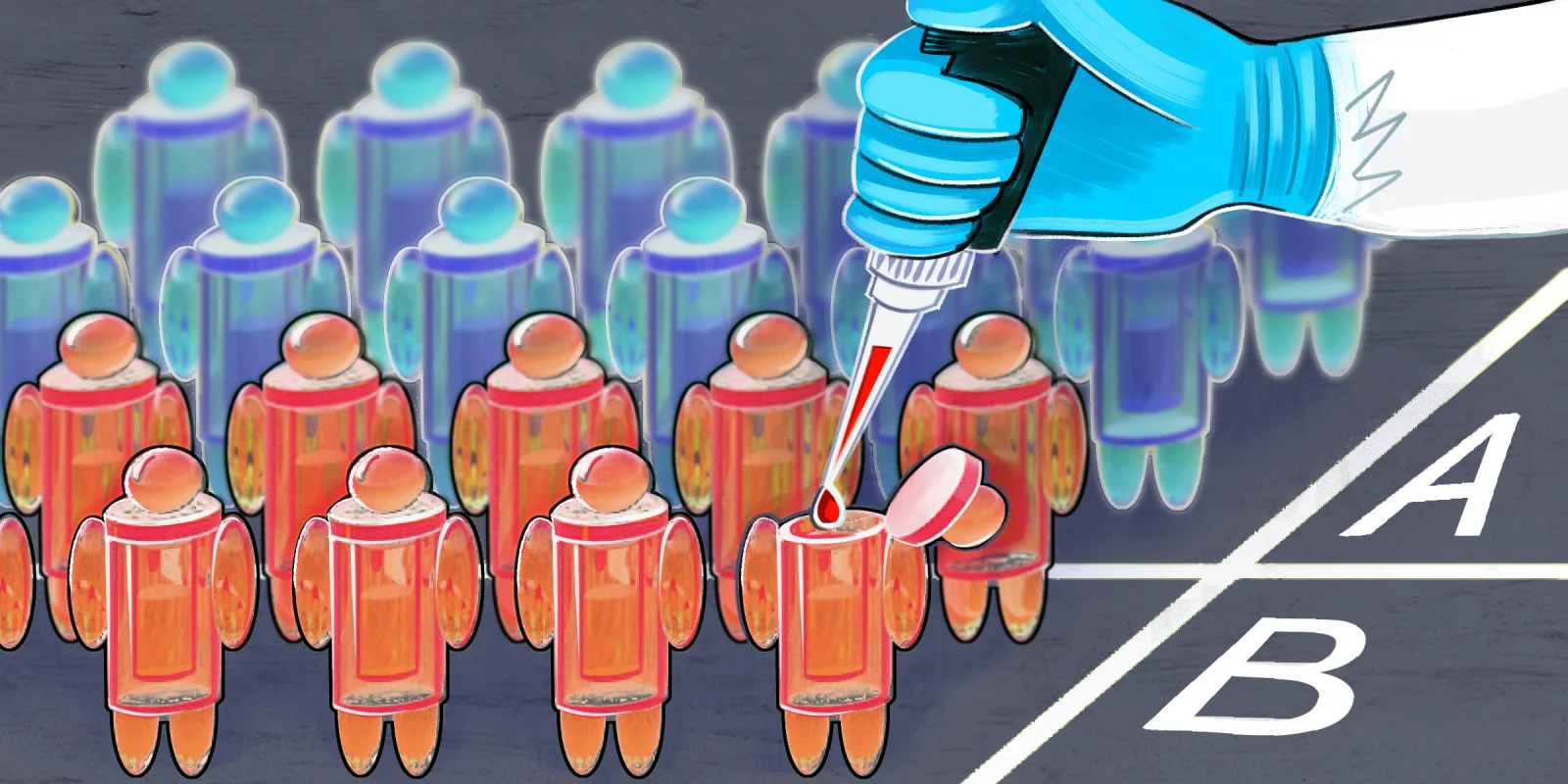
The trial design randomized 722 patients stratified by the International staging system stage and cytogenetic risk. Patients randomized to transplantation received three cycles of bortezomib lenalidomide dexamethasone, then had stem cell collection followed by immediate transplantation, followed by two cycles of bortezomib lenalidomide dexamethasone consolidation, followed by, finally, lenalidomide maintenance to progression. Patients in the non-transplant arm had stem cells collected but were not transplanted, receiving eight cycles of bortezomib lenalidomide dexamethasone so that the duration of induction was identical in both arms. Lenalidomide maintenance was also given until progression.
The patient's were well balanced in both arms. An important feature of this trial was this successful recruitment of underrepresented minorities frequently considered difficult to recruit subjects for clinical trials. Both arms had more than 18% Black patients enrolled.
The primary endpoint of the trial was progression-free survival. The median progression-free survival in the transplant arm was 67.5 months and in the non-transplant arm was 48.2 months. The 5 year progression-free survival was 55.6 and 41.5 months respectively. The hazard ratio was 1.53 favoring transplant. Similarly significant results were seen for time to progression and event free survival and points favoring transplantation. The benefit of transplantation was greatest for international stage I and least for international stage III patients. Patients with high risk genetics had the greatest benefit associated with transplantation with progression-free survival of 55.5 compared to 17.1 months. For patients with standard risk genetics the progression-free survivals were 82.3 and 53.2 months respectively favoring transplantation. Depth of response did not differ between the two arms even though the median duration of response was greater in the stem cell transplant on 56.4 versus 38.9 months. Overall survival was not different between arms at approximately 80 months.
The risk of therapy related myeloid neoplasm was 0 in the non-transplant arm, compared with 2.7% in the transplant arm. As expected, there was a decline in the quality of life in transplanted patients following conditioning but they recovered to baseline. Although all patients had stem cells collected, only 28% of the non-transplant arm had stem cell transplant as salvage therapy following the end of study.
This study’s conclusions indicate that transplants offer significantly superior progression-free survival with no overall survival benefit after median follow-up of over 6 years. The overall response rates were similar between the two arms. Fatal toxicity was seen in 1.6% of transplanted patients compared to 0.3% in non-transplanted patients.
With no overall survival differences, the utilization of transplantation may be personalized based on patient preferences. Application certainly is strongly advised in patients with high risk genetics.
Dr. Gertz reports no conflicts of interest.
Illustration by April Brust