In my third year of medical school, I spent one month on a busy obstetrics service. It was great fun because the faculty and residents allowed students to deliver a few babies. The experience caused tachycardia in the medical students, but after delivering the baby, clamping and cutting the umbilical cord, and handing the child to the mother; a sense of great accomplishment was assured. I was glad I had played lots of sports growing up; you need a sure set of hands because those new babies are slippery.
After medical school, I had not thought about delivering babies or anything to do with obstetrics. I am a surgical oncologist. The malignant or benign tumors I remove are a source of pain, angst, aggravation, and fear for my patients. After providing care for thousands of patients over the course of my career, it is rare to encounter something that startles me. But I can still be surprised and I enjoy a good practical joke, even when played on me.
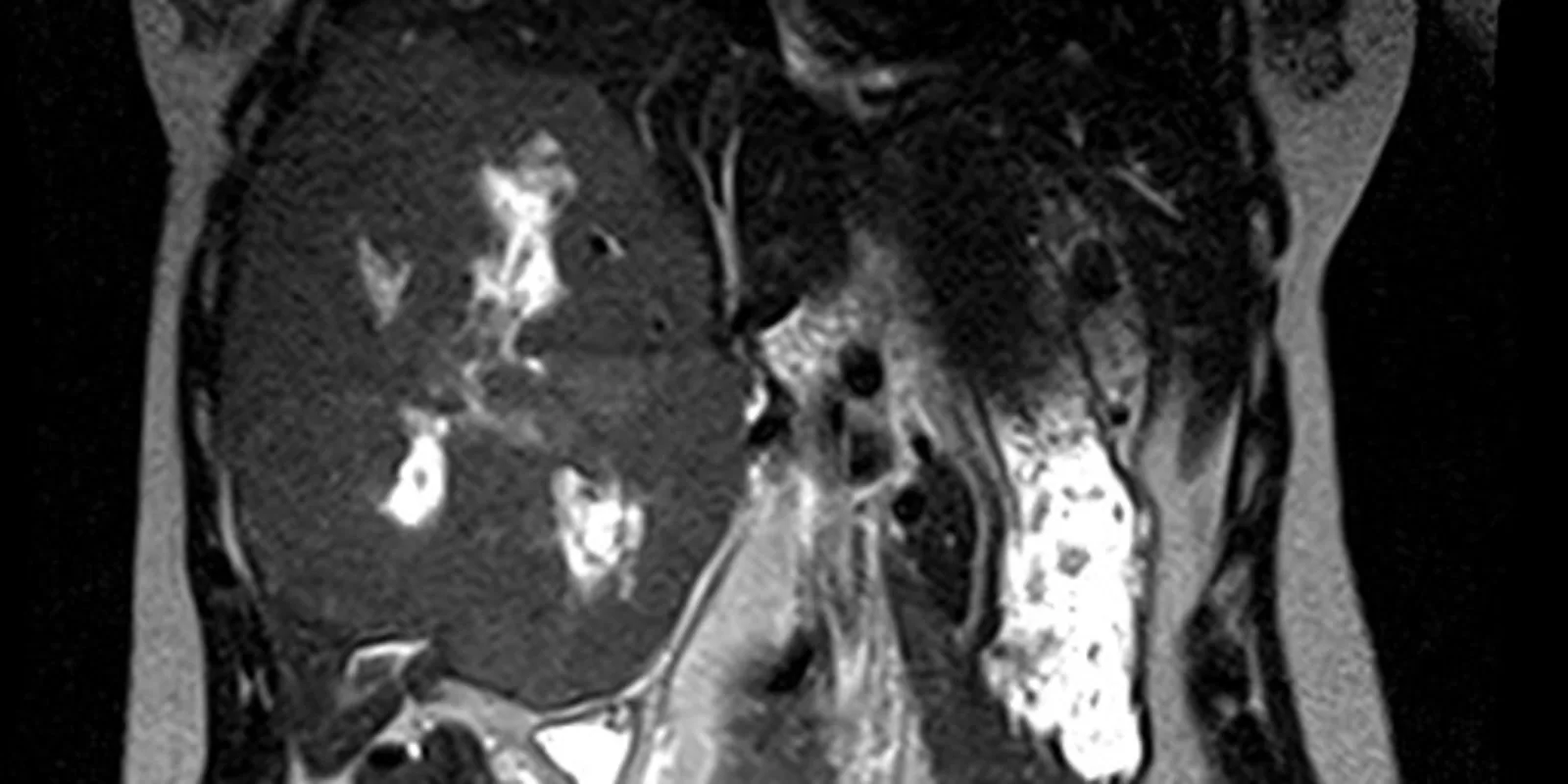
Several years ago a young woman not yet 30 years old was referred to me with a very large liver tumor. The patient had seen her local physician and reported she felt bloated and unable to eat a normal size meal. The referring physician was astonished to palpate a large abdominal mass. When I walked into the examination room to meet her, she stood and I wondered if she was pregnant. She had an obviously protuberant belly, and I soon learned why after viewing her magnetic resonance imaging (MRI).
An enormous tumor replaced the entire right lobe and medial segment of the left lobe of her liver. The MRI revealed a benign liver tumor called a giant cavernous hemangioma. The term giant was an understatement in this young lady. Hemangiomas are abnormal, but not malignant, spongy collections of blood vessels which can occur in many solid organs in the body.
This tumor was massive and clearly causing symptoms, so I recommended surgical removal. I knew the operation would be difficult because the right and middle hepatic veins were compressed and the tumor abutted and bowed the main, left, and right portal veins.
Liver surgeons use specialized pieces of equipment to dissect through the liver and expose blood vessels and bile ducts that can be clipped, tied, or stapled to prevent bleeding or bile leakage A surgical resident and I slowly and meticulously dissected through the liver, freeing the tumor from blood vessels and bile ducts. We proceeded through the liver until we identified and divided the final attachments; the right and middle hepatic veins. In a moment reminding me of the caesarean sections I had witnessed as a medical student, the resident and I wrestled the tumor out of the abdominal cavity, but, unlike the gentle swaddling of a newborn infant into a warm blanket, we indecorously plopped it into a large basin.
The patient recovered rapidly after her operation. She was young, healthy, walking the day after surgery, and quickly developed a ravenous appetite. Nothing like having a large tumor compressing your stomach and intestine removed to improve your interest in food again. The patient was discharged from the hospital four days after the operation.
I saw the patient back annually for a checkup to be certain she was doing well. Seven months after her 4-year visit I received an email from the patient requesting an urgent follow up appointment. Alarmed, I called my clinic staff to give her an appointment a few days later. When she arrived, I entered the examination room and was met by a somber-faced patient and her husband. She looked well but told me she had developed a new tumor. I asked if she was having symptoms similar to the liver tumor. She solemnly shook her head no. I inquired if she had a disk with MRI scans for me to see. Another shake of the head no, and then she said, “All I have is this.” She handed me a black and white ultrasound image.
I’ve been a surgical oncologist for 28 years, but thankfully my physical and mental facilities have not slowed. I studied the image for a few seconds, and when I looked up, my patient and her husband were grinning widely. She gleefully exclaimed, “I got you, didn’t I?”
Yes you did. The ultrasound image revealed a normal human fetus of fourteen weeks gestation. I’ve performed thousands of ultrasounds of the liver and pancreas, and while I’m not an obstetrician, I quickly recognized the image of a human fetus. After the laughter and general hilarity waned and I congratulated them for playing the scene (and me) perfectly, we had an excited discussion about the elation and tribulations of parenthood. I was thrilled for this young couple. This was not a conversation I had previously experienced in my practice.
A few weeks ago I noticed the patient’s name on my clinic schedule. I entered the exam room and was immediately introduced to her new son. I have delivered lots of tumors out of patients’ bodies over the course of my career, but this remarkable, alert, healthy delivery brought a smile of pure happiness to my face. Removing malignant tumors from patients is rewarding, challenging, and often provides the best chance for a patient to be cured of this dread disease. Even benign tumors can be problematic, symptomatic, and dangerous. We spent twenty minutes watching her newborn son while talking about the fatigue, sleeplessness, and fulfillment associated with an infant. She was tired, but triumphant. As she left, she waved and stated, “I could have never had him with that huge tumor inside me.”
It certainly would have been crowded in her abdominal cavity with both a giant liver tumor and a full term infant present. I’m glad the removal of the liver tumor went so well and she is fully living and enjoying life. And more importantly, she has now created new life and will experience all of the joy, pleasure, fatigue, frustration, and induction of gray hair associated with this phenomenon.